How to Get Free At-Home COVID-19 Tests
You can get four free tests from the government, and your insurer is required to cover up to eight tests per month. The devil is in the details.
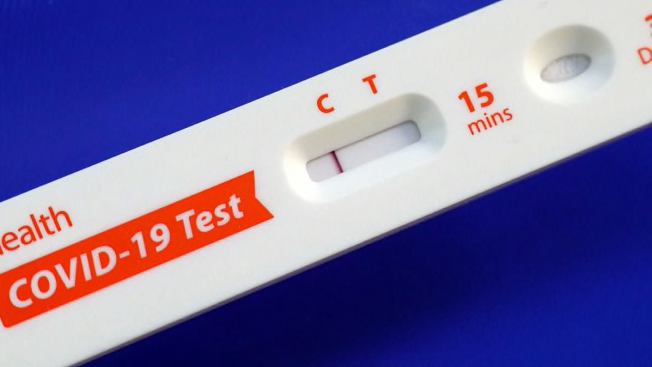
With the omicron variant sweeping across the U.S., many people are relying on testing to determine whether that sore throat is COVID-19 or that exposure at work led to an active infection. Until recently, at-home antigen tests like BinaxNow—which can help answer those questions quickly and easily—were expensive (generally at least $10 per test) and often out of reach.
Now, however, anyone in the U.S. can order a total of four free tests per household via COVIDtests.gov. The U.S. Postal Service will ship the tests directly to your door free of charge.
For people who need more tests, private health insurers are now required to cover the cost of up to eight at-home antigen tests per person per month, beginning with any tests purchased on or after Jan. 15. What exactly you have to do to get those tests at no cost to you will vary depending on your insurance plan. (PCR tests and rapid tests ordered or administered by a health provider continue to be fully covered by insurance.)
“There is a lot of confusion on how this initiative will roll out,” says Caitlin Donovan, a spokesperson for the National Patient Advocate Foundation in Washington, D.C. “So much of it is up to the individual health plans, and most are now scrambling to develop a strategy.”
Here’s what to know.
The Basics
The new federal rules give insurance companies a few options. If your insurer sets up a network of pharmacies and retailers, you should be able to pick up tests from one of them with no up-front costs. This may involve taking the tests to the pharmacy counter and checking out using your insurance card. If you buy tests from an out-of-network store, you can submit a reimbursement claim for up to $12 per test. If your insurer doesn’t set up a network of stores, it will be on the hook to reimburse you for the full cost of any covered tests.
How to Get a Covered Test
While the federal rules require insurers to cover up to eight tests per month, the specifics are left up to the individual insurance companies. That means consumers need to check with their health plan insurer to see exactly how it’s complying with the federal requirements. Check your insurer’s website; many have posted instructions or FAQs for finding covered tests or getting reimbursed for tests.
“How successful this new policy will be hinges on how quickly insurers can put processes in place to make it easy for consumers to buy at-home COVID-19 tests with no up-front costs,” says Katie Keith, principal of Keith Policy Solutions, a healthcare consultancy for foundations and nonprofits, and an adjunct professor of law at Georgetown University in Washington, D.C. “It will take a bit of time for this to all work out. It will be messy at the start.”
Initially, as insurers work to set up networks of online and in-person stores where members can pick up at-home test kits with no up-front costs, a more labor-intensive process will likely be more common: submitting receipts for reimbursement. Some pharmacy chains gave us statements indicating that they are in the process of working out details with certain insurance companies to allow customers to get free tests by showing their insurance card, but that in the meantime, people should expect to pay at the register for tests and submit claims for reimbursement.




















